What are nightmare bacteria and why are they worrying?
According to the latest report from the US Centers for Disease Control and Prevention (CDC), the number of cases of infections caused by "nightmare bacteria" has increased by nearly 70% over the past four years. These are strains of bacteria that are resistant to carbapenem, antibiotics are often considered the "last solution" in treating serious cases.
These resistant bacteria include Klebsiella pneumoniae and Escherichia coli, which do not respond to carbapenem treatment. In particular, the group of bacteria that produce the enzyme NDM (New Delhi metallo-beta-lactamase) causes most antibiotics to lose their effectiveness, making treatment extremely difficult.
Dr. Neha Rastogi Panda, an infectious disease expert at Fortis Memorial Research Institute (India), commented: "There are more and more patients traveling internationally and accessing medical services in many different countries, which contributes to promoting the rapid spread of drug-resistant bacteria".
In 2023 alone, the United States recorded more than 4,300 cases of NDM infections, five times more than in previous years. These cases have a high risk of death, especially in patients with weak immune systems or undergoing long-term treatment.
Causes of the increase and consequences
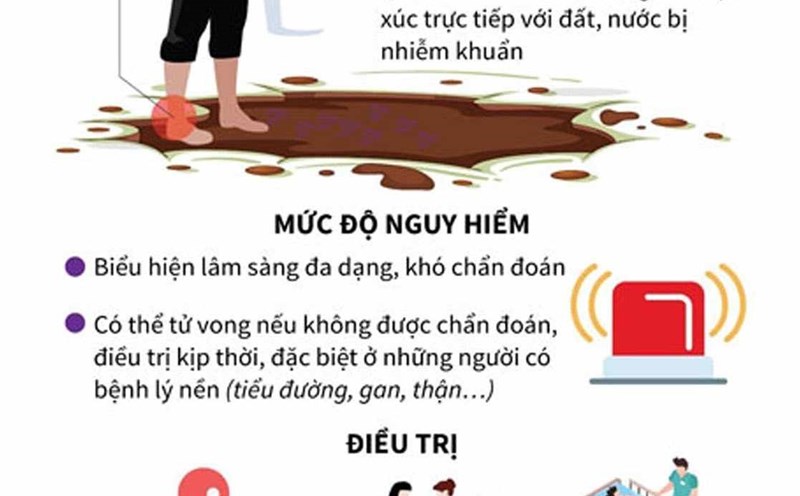
Experts say that antibiotic abuse in healthcare and agriculture, along with poor infection control at hospitals, is the main cause of this outbreak.
People with chronic diseases or weakened immune systems are at risk for more serious complications when infected with resistant bacteria, emphasizes Dr. Panda.
Some typical symptoms of nightmare bacterial infections include:
Urinary tract infections: urethra, urethra.
Blood infections: high fever, low blood pressure, heartbeat.
Pneumonia: cough, shortness of breath, chest pain.
We are seeing infections that do not respond to any conventional treatment, warned Dr Jonathan Smith, an infectious disease expert at Yale University. This is truly a race against time to develop new drugs.
Preventive solutions
In the context of increasing infections, the CDC calls on the community to take basic precautions:
Only take antibiotics when prescribed by a doctor.
Maintain personal hygiene and the living environment, especially in hospitals.
Monitor public health information, update epidemic warnings.
Scientists are also focusing on new-generation antibiotics and replacement therapies, but progress is still slow. While waiting, community responsibility in using antibiotics reasonably and raising awareness of disease prevention is the most effective measure.
As the CDC emphasizes: Nighterbed bacteria are no longer a far-reaching threat. They are present and fertile. Proactive prevention is our first line of defense".