Cerebral vascular malformations - Unpredictable danger in young people
Frequent headaches, sudden difficulty speaking, decreased vision, numbness in the limbs, etc. are symptoms that are easily confused with strokes, causing patients to be hospitalized during the "golden time". However, in many cases, doctors are still unable to save lives or if treated, the patient suffers severe sequelae. It is worth noting that the patients are often very young, some as young as 15 years old. The main cause is cerebral vascular malformations.
The 15-year-old patient was admitted to the hospital with a severe headache and quickly fell into a coma. At the lower-level hospital, the patient was diagnosed with a brain hemorrhage, intubated, and transferred to Bach Mai Hospital.
At the Stroke Center, the patient was in a deep coma, Glasgow score 5, dilated pupils, and a high fever of 39-40°C. The results of MSCT brain angiography showed bleeding in the thalamus and ventricles due to rupture of a cerebral arteriovenous malformation (AVM). Despite intensive resuscitation, the patient continued to deteriorate, with low blood pressure, deep coma, and death after two days of treatment.
In another case, a very young patient, 19 years old, healthy, suddenly had convulsions, deep coma and quadriplegia. MSCT scan results showed cerebral hemorrhage in the parieto-occipital lobe due to rupture of AVM (Spetzler-Martin point 3). After surgery to drain the hematoma and remove the malformation, the patient still had a limited prognosis and was treated in the Department of Surgical Intensive Care.
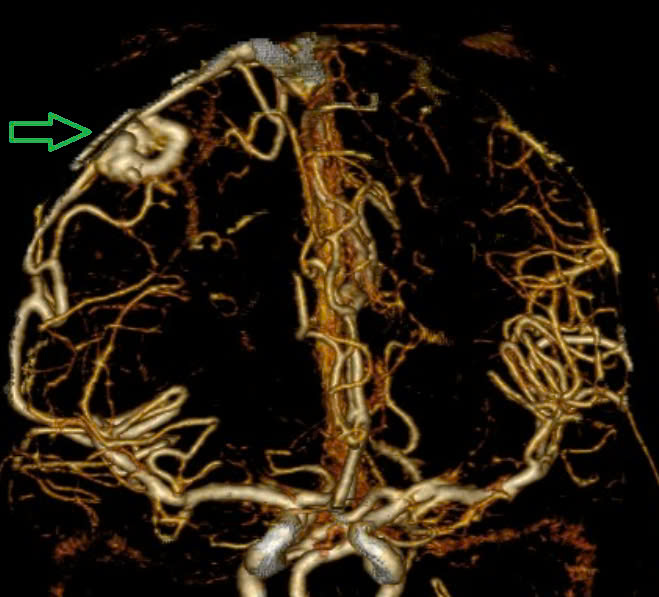
A 29-year-old female patient, previously healthy, was admitted to the hospital due to sudden headache, numbness in the hands, and severe vomiting. At Bach Mai Hospital, doctors determined that the patient had a right parietal lobe hemorrhage and a ruptured AVM (Spetzler-Martin point 2). After surgery and intensive treatment, the patient still suffered severe sequelae: complete paralysis of the left side of the body, and no awareness after a month.
The signs are often faint.
Dr. Le Tuan Anh - Stroke Center, Bach Mai Hospital said that cerebral arteriovenous malformation (AVM) is a congenital malformation of the vascular system. In the malformation, the artery connects directly to the vein without going through the capillaries, causing the vessel wall to become thin and the vein to dilate, with a very high risk of rupture. When ruptured, cerebral hemorrhage leads to increased intracranial pressure, seizures, loss of consciousness and rapid death.
AVMs often occur in young people, regardless of gender. The disease is difficult to detect if the malformation has not ruptured, and is only diagnosed incidentally through medical examination. Some signs that may occur when the malformation has not ruptured are headaches, dizziness, numbness in the limbs, or seizures. When ruptured, severe symptoms include severe headaches, vomiting, hemiplegia, confusion, deep coma, and even rapid death.
The mortality rate when AVM ruptures is estimated at 10-15%, with 50% of patients left with lifelong sequelae.
Doctors recommend: If you have symptoms of headache, dizziness, numbness in the limbs, or convulsions, you should see a doctor soon. If you suddenly lose consciousness, you should go to the hospital immediately for timely treatment. Early detection of cerebral vascular malformations can reduce the risk of complications and death.
A brain arteriovenous malformation is an abnormal connection between arteries and veins in the body. Arteries are responsible for transporting oxygen-rich blood from the heart to the brain. Veins carry oxygen-depleted blood back to the lungs and heart. When an arteriovenous malformation occurs in the brain, this important process is disrupted.
Cerebral arteriovenous malformations account for approximately 2% of all hemorrhagic strokes each year and are often the cause of bleeding in children and young adults with intracerebral hemorrhage.